Vector-Borne Diseases
Diseases that are transmitted by vectors are generally referred to as vector-borne diseases. A vector is any animal or insect that is capable of transmitting a pathogen. The term vector-borne disease includes arboviruses (arthropod-borne viruses), mosquito-borne diseases, tick-borne diseases, flea-borne diseases, and others. Vectors must be infected by a pathogen before they are capable of transmitting the pathogen to people or animals.
Click to jump to section.
Public Health Concerns
Currently, West Nile Virus (WNV) and St. Louis Encephalitis virus (SLEV) are the mosquito-borne diseases of greatest concern to District residents. Every summer, these two viruses infect birds, mosquitoes and people across the United States. Western Equine Encephalomyelitis virus (WEEV) has not been detected in California for several years but mosquito and bird samples are regularly tested to ensure this virus has not reemerged in the District.
New health threats in the form of Zika, Dengue, and Chikungunya are of greater concern to travelers but, with the arrival of the invasive Aedes aegypti mosquito to the District, have a risk of being transmitted locally.
Mosquito traps only catch mosquitoes that are already in the general area of the mosquito trap. While there are many types of traps, Delta Vector Control District uses three main types for their surveillance.
West Nile Virus
West Nile Virus (WNV) is the most common mosquito-borne disease in the District and across the United States. It is spread to people through the bite of an infected mosquito. Roughly 20% of people infected with West Nile Virus will develop symptoms such as fever, headache, and nausea. Less than 1% of infected people will become very sick after the virus affects the brain or nervous system. Symptoms of neuroinvasive West Nile Virus may include neck stiffness, vision loss, numbness, paralysis, and even death. Symptoms may last for several weeks or be permanent. Although symptoms typically appear within 3 to 14 days after being bitten by an infected mosquito, it may take longer to appear in individuals with certain medical conditions.
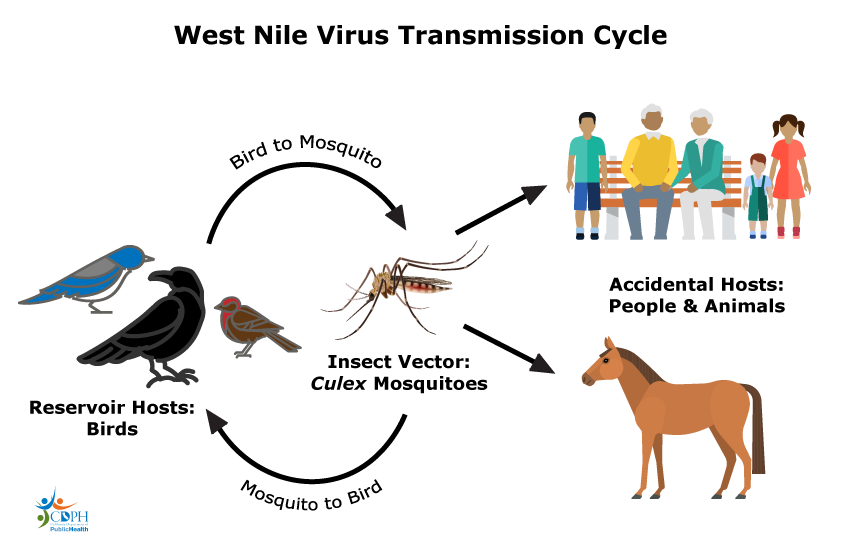
Transmission Cycle
Wild birds are the reservoir host for West Nile Virus. Reservoir hosts are humans or animals where a pathogen normally lives, grows, and multiplies. There are over 200 bird species that are capable of carrying West Nile Virus. Some bird species, once infected, will develop very high levels of virus that can then be spread to mosquitoes that bite them.
Culex mosquitoes are the main vector for West Nile Virus. This is because Culex mosquitoes generally prefer to feed on birds. Mosquitoes become infected when they feed on an infected bird. Once infected, these mosquitoes can spread West Nile Virus to humans, birds, and other animals through their bite.
West Nile Virus is not spread person to person by mosquitoes. People and animals are accidental hosts for the virus. Accidental hosts will not produce enough virus in their blood to continue the transmission cycle if they get bitten by an uninfected mosquito. Blood donations are screened for West Nile Virus.
Who is most at risk?
Anyone can be infected by West Nile Virus through the bite of an infected mosquito and become ill. However, certain groups of people have a higher risk of developing severe illness and should take extra precautions to avoid mosquito bites. These groups include people:
- Over the age of 60 years
- With weakened immune systems
- With diabetes, kidney disease, or some other medical condition
See your medical provider if you think you may have West Nile Virus.
Prevention
There are no effective medical treatments or human immunizations for West Nile Virus. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections.
- Prevent mosquito bites by using an EPA-registered insect repellent with DEET, picaridin, IR3535, or oil of lemon eucalyptus before you go outside.
- Avoid spending time outdoors around dawn and dusk or take extra precautions to avoid bites during this time. Culex mosquitoes, the vector for West Nile Virus, are most active at dawn and dusk.
- Install window and door screens that fit tightly into their frames. Check for and repair any holes or tears you find.
- Dump standing water around your yard at least once a week. Request free mosquitofish or anonymously report neglected swimming pools here.
Visit our Prevention page to learn more about source reduction and bite prevention.
Animals and WNV
Other animals can be infected with West Nile Virus if they are bitten by an infected mosquito. However, most animals will not get sick. West Nile Virus can cause severe illness in birds, tree squirrels, and horses.
While many bird species can carry West Nile Virus, some species like crows, ravens, jays and magpies can become very ill and die. Bird die offs can be an indicator that West Nile Virus is in the area. Tree squirrels infected with WNV can develop symptoms including shaking, circling, or paralysis and may die. You can report dead birds or tree squirrels directly to the District at 559-732-8606 during regular business hours or through the California West Nile Virus Hotline online at www.westnile.ca.gov or by calling 1-877-968-2473. If the dead bird or squirrel meets the criteria for disease testing, someone will contact you to arrange a pick up.
Horses infected with West Nile Virus may develop symptoms such as fever, stumbling, muscle twitching, and reduced appetite. The fatality rate for horses showing symptoms is roughly 33%. Horses that recover may have long term side effects including behavioral issues and problems with their gait. A West Nile Virus vaccine is available for horses and is strongly recommended. Cats and dogs can be infected by West Nile Virus but they rarely get sick.
Contact your veterinarian for more information.
St. Louis Encephalitis Virus
Saint Louis Encephalitis Virus (SLEV) is a mosquito-borne disease that can cause inflammation of the brain. In the District, it is less common than West Nile Virus but is typically detected in mosquitoes every summer. It is spread to people through the bite of an infected mosquito. Mosquitoes become infected when they feed on an infected bird. Less than 1% of people infected will develop mild, flu-like symptoms within 5 to 15 days of being bitten. Some people may develop more severe symptoms when the virus infects the central nervous system. These symptoms include stiff neck, convulsions, paralysis, coma, and even death. St. Louis Encephalitis Virus infections tend to be more severe in older adults than in children.
See your medical provider if you think you may have St. Louis Encephalitis Virus.
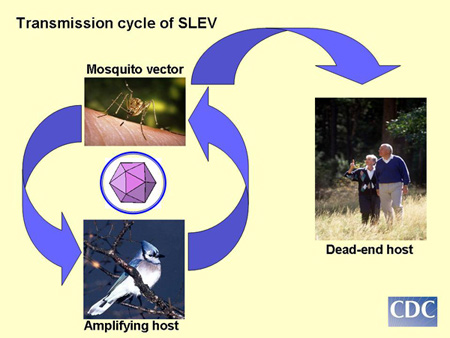
Transmission Cycle
Wild birds are the reservoir host for St. Louis Encephalitis Virus. Reservoir hosts are humans or animals where a pathogen normally lives, grows, and multiplies. Some bird species, once infected, will develop very high levels of virus that can then be spread to mosquitoes that bite them. Birds become infected when an infected mosquito bites them.
Culex mosquitoes are the main vector for St. Louis Encephalitis Virus. This is because Culex mosquitoes generally prefer to feed on birds. Mosquitoes become infected when they feed on an infected bird. Once infected, these mosquitoes can spread St. Louis Encephalitis Virus to humans, birds, and other animals through their bite.
St. Louis encephalitis Virus is not spread person to person by mosquitoes. People are accidental hosts for the virus. Accidental hosts will not produce enough virus in their blood to continue the transmission cycle if they get bitten by an uninfected mosquito.
Who is most at risk?
Anyone can be infected by St. Louis Encephalitis Virus through the bite of an infected mosquito and become ill. However, the elderly and those with weakened immune systems have a higher risk of developing severe illness and should take extra precautions to avoid mosquito bites.
Prevention
There are no effective medical treatments or human immunizations for St. Louis Encephalitis Virus. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections.
- Prevent mosquito bites by using an EPA-registered insect repellent with DEET, picaridin, IR3535, or oil of lemon eucalyptus before you go outside.
- Avoid spending time outdoors around dawn and dusk or take extra precautions to avoid bites during this time. Culex mosquitoes, the vector for St. Louis Encephalitis Virus, are most active at dawn and dusk.
- Install window and door screens that fit tightly into their frames. Check for and repair any holes or tears you find.
- Dump standing water around your yard at least once a week. Request free mosquitofish or anonymously report neglected swimming pools here.
Visit our Prevention page to learn more about source reduction and bite prevention.
Animals and WNV
Many wild bird species can carry St. Louis Encephalitis Virus without getting sick. You can report dead birds directly to the District at 559-732-8606 during regular business hours or through the California West Nile Virus Hotline online at www.westnile.ca.gov or by calling 1-877-968-2473. If the dead bird meets the criteria for disease testing, someone will contact you to arrange a pick up.
Most other animals infected with St. Louis Encephalitis Virus do not become sick. Contact your veterinarian for more information if you are concerned about your pet.
Western Equine Encephalomyelitis Virus
Western Equine Encephalomyelitis Virus (WEEV) is a mosquito-borne disease that can cause inflammation of the brain. It is spread to people through the bite of an infected mosquito. Mosquitoes become infected when they feed on an infected bird.
Although it has not been detected in California for several years, WEEV was an important cause of illness and death in humans and horses in the past. Human cases are very rare. Most people infected with WEEV will have no symptoms or a mild flu-like illness that develops within 5 to 15 days after being bitten by an infected mosquito. A small percentage of people may develop more severe symptoms including stiff neck, vomiting, weakness, seizures, coma, and even death. The risk of severe disease is higher in very young children and older adults.
Transmission Cycle
Wild birds are the reservoir host for Western Equine Encephalomyelitis Virus. Reservoir hosts are humans or animals where a pathogen normally lives, grows, and multiplies. Some bird species, once infected, will develop very high levels of virus that can then be spread to mosquitoes that bite them. Birds become infected when an infected mosquito bites them.
Culex mosquitoes are the main vector for Western Equine Encephalomyelitis Virus. This is because Culex mosquitoes generally prefer to feed on birds. Mosquitoes become infected when they feed on an infected bird. Once infected, these mosquitoes can spread Western Equine Encephalomyelitis Virus to humans, birds, and other animals through their bite.
Western Equine Encephalomyelitis Virus is not spread person to person by mosquitoes. People and animals are accidental hosts for the virus. Accidental hosts will not produce enough virus in their blood to continue the transmission cycle if they get bitten by an uninfected mosquito.
Who is most at risk?
Anyone can be infected by Western Equine Encephalomyelitis Virus through the bite of an infected mosquito and become ill. However, very young children and the elderly have a higher risk of developing severe illness and should take extra precautions to avoid mosquito bites.
Prevention
There are no effective medical treatments or human immunizations for Western Equine Encephalomyelitis Virus. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections.
- Prevent mosquito bites by using an EPA-registered insect repellent with DEET, picaridin, IR3535, or oil of lemon eucalyptus before you go outside.
- Avoid spending time outdoors around dawn and dusk or take extra precautions to avoid bites during this time. Culex mosquitoes, the vector for Western Equine Encephalomyelitis Virus, are most active at dawn and dusk.
- Install window and door screens that fit tightly into their frames. Check for and repair any holes or tears you find.
- Dump standing water around your yard at least once a week. Request free mosquitofish or anonymously report neglected swimming pools here.
Visit our Prevention page to learn more about source reduction and bite prevention.
Animals and WNV
Many wild bird species can carry Western Equine Encephalomyelitis Virus without getting sick. You can report dead birds directly to the District at 559-732-8606 during regular business hours or through the California West Nile Virus Hotline online at www.westnile.ca.gov or by calling 1-877-968-2473. If the dead bird meets the criteria for disease testing, someone will contact you to arrange a pick up.
Horses that are infected with Western Equine Encephalomyelitis Virus may develop symptoms such as fever, stumbling, muscle twitching, and reduced appetite. The fatality rate for horses showing symptoms is between 15-30%. Horses that recover may have long term side effects including behavioral issues and problems walking. A Western Equine Encephalomyelitis Virus vaccine is available for horses and is strongly recommended.
Contact your veterinarian for more information if you are concerned about your horse.
New and Emerging Health Risks
In 2014, the invasive Aedes aegypti mosquito was found in Exeter, bringing new mosquito-borne disease threats to the District. Invasive Aedes mosquitoes are capable of transmitting different viruses than the native mosquito species. Once infected, Aedes aegypti mosquitoes can spread Zika, dengue, chikungunya, and yellow fever virus through their bite.
There is currently no local transmission of these viruses in California. Local transmission may occur if the Aedes aegypti from this area bite people who are infected. This may happen when someone does not realize they have been infected after traveling to an area with local transmission. Mosquito control and bite prevention can prevent local transmission from occurring in our District.
Zika
Zika is a mosquito-borne disease that can cause birth defects in newborns and is associated with Guillain-Barré Syndrome, a disease affecting the nervous system, in adults. Although Zika is primarily spread through the bite of an infected mosquito, it can also be transmitted from a pregnant woman to her developing baby and through unprotected sex. Mosquitoes become infected when they bite a person who has Zika virus in their blood.
Most people who are infected with Zika do not develop any symptoms. A small percentage of people may develop fever, rash, joint pain, and/or red eyes. Zika is a serious risk to a pregnant woman’s developing baby and may cause miscarriage, still birth, or severe birth defects.
There is no effective medical treatment or human immunization available for Zika. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections. Contact your healthcare provider if you believe you may have Zika or if you or your partner are pregnant, or planning to become pregnant, while traveling to an area with local Zika transmission. Continue to avoid mosquito bites for 3 weeks after traveling to an area with Zika.
For more information, please visit Zika 101 from the California Department of Public Health. Contact your healthcare provider if you believe you may have Zika.
Dengue
Dengue is a mosquito-borne disease that is caused by dengue virus 1, 2, 3, or 4. It is spread through the bite of an infected Aedes aegypti or Aedes albopictus mosquito. These mosquitoes become infected when they bite a person who has dengue virus in their blood. Pregnant women can transmit dengue to their child during the pregnancy or around the time of birth.
About 25% of people with dengue will develop a fever, headache, pain behind the eyes, rash, joint pain, bone pain, or muscle pains. Of those who get sick, about 1 in 20 will develop severe dengue. Symptoms of severe dengue can develop within a few hours and include stomach pain or tenderness, vomiting, respiratory distress, internal bleeding, shock, and even death. Severe dengue is a medical emergency.
There is no effective medical treatment for dengue. A dengue vaccine is available for people living in certain areas of the world who have had a confirmed prior dengue infection. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections. Continue to avoid mosquito bites for 3 weeks after traveling to an area with dengue.
Contact your healthcare provider if you believe you may have dengue.
Chikungunya
Chikungunya is a mosquito-borne disease that is spread through the bite of an infected Aedes aegypti or Aedes albopictus mosquito. These mosquitoes become infected when they bite a person who has chikungunya virus in their blood.
Most people infected with chikungunya virus will develop symptoms within a week of being bitten by an infected mosquito. Symptoms may include fever, joint pain, joint swelling, headache, and rash. These symptoms may be severe and disabling with joint pain lasting months. Newborns, people over the age of 65 years, and people with medical conditions have a greater risk for more severe disease.
There is no vaccine or medical treatment available for chikungunya. Preventing mosquito bites and reducing mosquito populations is the best approach to preventing infections. Continue to avoid mosquito bites for 3 weeks after traveling to an area with chikungunya.
Contact your healthcare provider if you believe you may have chikungunya.
Yellow Fever
Yellow fever is a mosquito-borne disease that is spread through the bite of an infected Aedes aegypti or Aedes albopictus mosquito. These mosquitoes become infected when they bite a person who has yellow fever virus in their blood.
Most people who are infected with yellow fever virus will not develop symptoms. For those that do, symptoms will typically appear within 3 to 6 days and include fever, chills, headache, back pain, body aches, nausea, vomiting, and fatigue. About 1 in 7 people will develop a more severe illness that includes jaundice (yellow skin), bleeding, organ failure, shock, and death. Between 30% to 60% of people who develop severe illness will die.
There is no medicine to treat or cure a yellow fever infection. A vaccine is available that prevents yellow fever. If you are traveling to an area where yellow fever is endemic, being vaccinated is highly recommended. Preventing mosquito bites can help prevent infections. Continue to avoid mosquito bites for 3 weeks after traveling to an area with yellow fever.
Contact your healthcare provider if you believe you may have yellow fever or before traveling to an area where yellow fever is endemic.
Tick-borne Disease
There are 6 species of ticks in California that are known to bite people. These ticks can sometimes carry pathogens that they can transmit to people through their bite. These pathogens include Lyme disease, babesiosis, anaplasmosis, tularemia, spotted fever, and tick paralysis. Of these, Lyme disease is the most common tick-borne disease in California, distantly followed by tick-borne relapsing fever, tularemia, and spotted fever. The others are very rare.
Symptoms of tick-borne illness typically start within 30 days of being bitten by an infected tick and can vary widely, from mild illness to death. Symptoms may include fever, rash, headache, muscle pain, or joint swelling and pain. Contact your healthcare provider if you develop any of these symptoms after being bitten by a tick.
Avoiding tick bites is the best way to prevent tick-borne diseases.
Lyme Disease
Lyme disease can start with flu-like symptoms and develop into severe, chronic joint and nervous system problems over time. Symptoms of Lyme disease typically appear within 30 days of being bitten by a tick. Early symptoms may include fever, headache, swollen lymph nodes, skin rash, heart irregularities, or muscle and joint pain. If untreated, some people with Lyme disease may develop pain and swelling in their joints, especially the knees and numbness, tingling, or pain in the extremities along with difficulty concentrating and memory problems.
If you develop any symptoms within 30 days of being bitten by a tick, contact your healthcare provider. Antibiotics can successfully treat Lyme disease, especially in the early stages. For more information about Lyme disease, visit the Lyme Disease page from the California Department of Public Health or from the Centers for Disease Control and Prevention.
Tick-Borne Relapsing Fever
Tick-borne relapsing fever is a bacterial disease that can be spread to people through the bite of an infected soft tick. Soft ticks are mostly found in forested mountain and foothill areas where they can easily feed on rodents, their preferred meal choice. These ticks typically live in rodent nests, wood piles, under floorboards, and cracks and crevices.
People infected with tick-borne relapsing fever typically develop symptoms about a week after being bitten by an infected tick. Symptoms may include a sudden high fever (104-105 F), chills, headache, muscle aches, nausea, vomiting, abdominal pain, or a rash. The symptoms occur in cycles, lasting between 3-5 days before disappearing for a few days, then occurring again.
If you develop any symptoms within 30 days of being bitten by a tick, contact your healthcare provider. Antibiotics can successfully treat tick-borne relapsing fever and people rarely develop chronic health problems or die. For more information about tick-borne relapsing fever, visit the California Department of Public Health website.
Tularemia
Tularemia is a bacterial disease that can be transmitted to people through the bite of an infected Pacific coast tick (Dermacentor occidentalis), American dog tick (Dermacentor variabilis), or deerfly (Chrysops discalis). People are most commonly infected through direct contact with an infected wild animal. Wild rabbits are the most common source of infection. People can also become infected if they eat meat from an infected animal.
People who are infected with tularemia may develop a severe illness or even death. Symptoms typically appear about 3 to 5 days after infection and may include chills, fever, headache, body aches, cough, and pain or tightness in the chest. Lymph nodes in the neck, underarms, or groin may be swollen and painful. The bite or wound site may form an ulcer. If left untreated, tularemia bacteria can cause pneumonia, blood infection, conjunctivitis, or meningitis.
To prevent tularemia, avoid touching or handling animal carcasses. Use gloves when wild game meat and cook thoroughly before eating. Use an EPA registered insect repellent to prevent tick bites and check for ticks frequently.
If you develop any symptoms after handling a wild animal, especially rabbits, or being bitten by a tick, contact your healthcare provider. Antibiotics can successfully treat tularemia. For more information about tularemia, visit the California Department of Public Health or the Centers for Disease Control and Prevention website.
Spotted Fever Group Rickettsia
The Spotted Fever Group Rickettsia are a group of bacterial diseases that are associated with a rash and that are transmitted through the bite of an infected tick. They include Rocky Mountain Spotted Fever and Pacific Coast Tick Fever. Pacific Coast Tick Fever is transmitted through the bite of an infected Pacific coast tick (Dermacentor occidentalis), while Rocky Mountain Spotted Fever can be spread through the bite of an infected American dog tick (Dermacentor variabilis), Pacific coast tick (Dermacentor occidentalis), or brown dog tick (Rhipicephalus sanguineus).
Symptoms of Rocky Mountain Spotted Fever typically occur between 2 to 14 days after being being by an infected tick. Symptoms can include fever followed by weakness, muscle pain, severe headache, and a painful abdomen. Some people may develop a rash that covers most of the body including the palms of the hands and soles of the feet. If not treated, the fever can last for two to three weeks and lead to other symptoms, such as weakness, deep muscle pain, severe headache, chills, blood-shot eyes, and a painful abdomen. Kidney failure and even death may result in severe cases. Pacific Coast Tick Fever causes similar but milder symptoms with the addition of a small, open wound that turns into a dark scab.
If you develop any symptoms within 30 days of being bitten by a tick, contact your healthcare provider. Antibiotics can successfully treat infections form the spotted fever group Rickettsia. Left untreated, up to 25% of people infected with Rocky Mountain Spotted Fever may die. For more information, visit the California Department of Public Health website or the Centers for Disease Control and Prevention RMSF page or Other Spotted Fever Group page.
Prevention
Avoiding tick bites can reduce your risk of developing a tick-borne disease.
- Use an EPA-registered repellent for use against ticks such as those with at least 20% DEET. Visit the EPA Repellent Search Tool to find a repellent that is right for you.
- Before hikes, treat clothing with permethrin to kill ticks.
- Stay in the middle of trails when hiking or walking. Avoid walking through grassy areas, sitting on logs, tree trunks, or other vegetation.
- Keep grass mowed along trails, buildings, camping, and other outdoor gathering areas.
- Check yourself, others, and pets for ticks during and up to 3 days after outdoor activities such as hiking.
- Shower soon after returning from outdoor activities in tick habitat.
- Place clothes worn during outdoor activities in a hot dryer for 10 minutes before washing.
If you are bitten, promptly removing the tick can help prevent disease transmission.
- Grasp the tick’s mouthparts with tweezers as close to the skin as possible.
- Pull the tick straight out using a gentle, steady motion. Avoid twisting or jerking the tick which can cause the mouthparts to break off in the skin.
- Wash the bite site and your hands with soap and water.
Contact your healthcare provider if you develop any symptoms within 30 days of being bitten by a tick.
Threats to Pets & Domestic Animals
Mosquitoes and ticks can spread pathogens to domestic animals and pets through their bite. However, not all animals will get sick after being bitten. Whether an animal gets sick depends on the type of animal as well as the pathogen.
Dog Heartworm
Dog heartworm is a roundworm species that can be transmitted to dogs through the bite of an infected mosquito. Mosquitoes become infected when they feed on a sick dog. Aedes sierrensis mosquitoes are the main mosquito species that transmits dog heartworm in California.
Once infected, dogs can become very sick if left untreated. Treatments can help control the infection in your pet but will not cure it. Prevention is the best option to protect your pet from dog heartworm. Talk to your veterinarian for prevention options and practice weekly source reduction around your yard to help reduce mosquito populations.
Encephalitis in Horses
Horses can be infected by West Nile Virus and Western Equine Encephalomyelitis Virus if they are bitten by an infected mosquito. Mosquitoes become infected after biting an infected bird. These viruses can cause severe illness and even death in horses.
Every year, West Nile Virus is detected in mosquitoes in the District. Western Equine Encephalomyelitis Virus has not been detected in California for several years. Eastern Equine Encephalitis Virus and Venezuelan Equine Encephalitis Virus can also be spread to horses through the bite of an infected mosquito and cause severe illness but these viruses have been detected in the District.
Infected horses may develop only a mild illness or more severe symptoms. Symptoms may include fever, stumbling, muscle twitching, reduced appetite, and even death. Horses that recover may have long term side effects including behavioral issues and problems walking. A vaccine for West Nile, Western Equine Encephalomyelitis, and Eastern Equine Encephalitis virus is available for horses and is strongly recommended.
Contact your veterinarian for more information if you are concerned about your horse.
Tick-borne Diseases in Pets & Horses
Dogs, cats, and horses are at risk for several tick-borne infections including Lyme disease, tularemia, ehrlichiosis, babesiosis, and others. Tick-borne pathogens are transmitted through the bite of an infected tick. Symptoms of tick-borne diseases can vary widely depending on the type of pathogen as well as the animals. Many animals will not show symptoms while others may become very ill or even die.
Pets that spend time in grassy, wooded, or brushy areas are at a higher risk for tick bites. Treating your pets for ticks and removing them promptly can help prevent tick-borne diseases. Talk to your veterinarian to discuss options to prevent ticks.
Horses
Lyme disease, tularemia, and anaplasmosis are common tick-borne diseases that horses can get through the bite of an infected tick. Horses may develop a wide range of symptoms including fever, loss of appetite, discoloration of mucous membranes, and swelling of the legs, the underside of the chest, or abdomen.
Removing ticks promptly can help reduce the risk of tick-borne diseases in horses. Check for ticks around the tail, ears, and eyes as well between the back legs and under the front legs. Talk to your veterinarian about options to treat for ticks.
Dogs
Dogs may be at risk for Rocky Mountain spotted fever (RMSF), ehrlichiosis, and Lyme disease. These are bacterial infections that can be transmitted through the bite of an infected tick. Removing ticks promptly can reduce the risk of disease transmission. Fever and lameness or stiffness is a common sign of a tick-borne infection in dogs. Other symptoms may include coughing, lack of energy, loss of appetite, and swelling of the lymph nodes, joints, legs, or face.
Talk to your veterinarian about treatment options to prevent tick bites. Removing ticks promptly can help reduce the risk of disease transmission. Check your dog for ticks between the legs and toes, under collars, and around the ears and the eyes.
Cats
Cats may show a wide variety of symptoms from tick-borne infections. Cats may have ticks in and around the ears, around the eyelids, under collars, under front legs, between the back legs, between the toes, or around the tail. Remove ticks from pets promptly to reduce disease risk.
Cats can be very sensitive to different chemical treatments for ticks. Always talk to your veterinarian before applying a tick treatment to your cat.
Plague (Yersinia pestis)
Plague is a rare but serious bacterial disease that is most commonly transmitted through the bite of infected fleas. However, people can also become infected by touching an animal that is infected with plague or by inhaling infectious droplets that a sick animal has coughed into the air. Fleas become infected after biting an infected rodent or small animal. Dogs and cats can also become infected after eating infected rodents or other infected small animals.
Although dogs are unlikely to develop noticeable illness if infected, cats with plague can become very sick. Symptoms can include fever, loss of appetite, swollen lymph nodes on the neck, pneumonia, cough, or difficulty breathing. Dogs, cats, rodents, and other small animals that are infected with plague can spread the infection to humans that handle them. Owners should contact their veterinarian as soon as possible and reduce contact with the sick animal to decrease the risk of infection.
People and pets in the western United States, especially in rural areas, may be at increased risk. Those who handle animals such as hunters or people who sleep with pets may have a higher risk as well. Reduce potential exposure to fleas and bodily fluids of infected animals can reduce the risk of transmission. Contact your veterinarian for flea treatment options for your pet.
Cats can be very sensitive to different chemical treatments for fleas. Always talk to your veterinarian before applying a flea treatment to your cat.
Service Request? Get in Touch.
Public Documents
Contact
1737 West Houston Ave
Visalia, CA. 93291
Ph. 559-732-8606
TF. 877-732-8606
Fax. 559-732-7441
Hours
Monday–Friday,
7:30 AM to 4:00 PM (excluding holidays)